Infectious Diseases | Pathophysiology of Viral Hepatitis
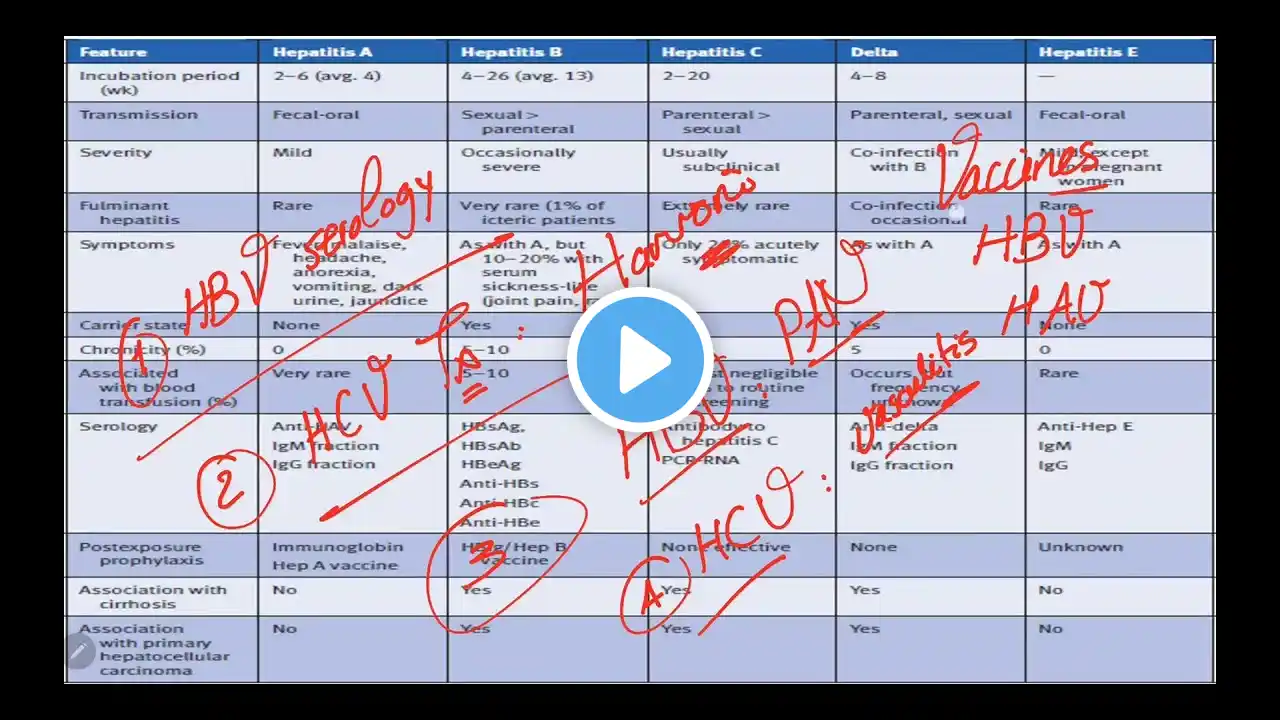
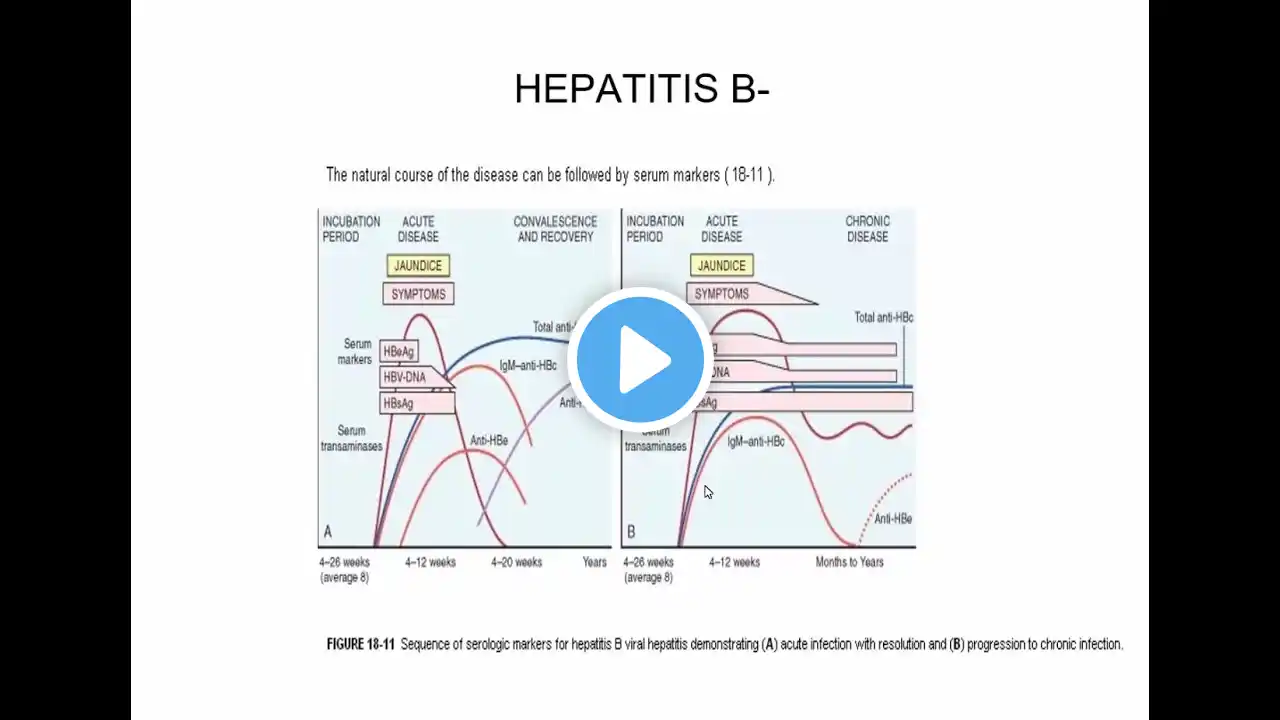
Introduction to Viral Hepatitis Viral hepatitis refers to a group of liver infections caused by different viruses. The most common types are hepatitis A, B, C, D, and E. These infections can lead to both acute and chronic liver disease, with varying degrees of severity and potential complications. Types of Hepatitis Viruses 1. *Hepatitis A Virus (HAV):* *Transmission:* Fecal-oral route, often through contaminated food or water. *Pathophysiology:* HAV infects hepatocytes, leading to an inflammatory response. The liver damage is primarily immune-mediated as the body's immune cells attack infected hepatocytes. HAV typically causes an acute infection that the body clears, leading to lifelong immunity. 2. *Hepatitis B Virus (HBV):* *Transmission:* Blood and body fluids, including perinatal (from mother to child at birth), sexual contact, and needle sharing. *Pathophysiology:* HBV infects hepatocytes and integrates into the host's DNA in chronic cases. The immune response to HBV-infected cells leads to inflammation and liver cell death. 3. *Hepatitis C Virus (HCV):* *Transmission:* Bloodborne, primarily through needle sharing and, less commonly, through sexual contact and from mother to child at birth. *Pathophysiology:* HCV directly infects hepatocytes, leading to a chronic infection in the majority of cases. The chronic immune response against infected cells results in ongoing inflammation, fibrosis, cirrhosis, and a significant risk of liver cancer. 4. *Hepatitis D Virus (HDV):* *Transmission:* Blood and body fluids, often requires co-infection with HBV. *Pathophysiology:* HDV is a defective virus that requires HBV for its replication. Co-infection with HBV and HDV tends to cause more severe liver disease than HBV alone, including a higher risk of cirrhosis and liver cancer. 5. *Hepatitis E Virus (HEV):* *Transmission:* Fecal-oral route, often through contaminated water. *Pathophysiology:* HEV infection is similar to HAV, causing an acute hepatitis. It is usually self-limiting but can be severe in pregnant women and immunocompromised individuals. Pathophysiology Overview 1. *Entry and Initial Infection:* The hepatitis viruses enter the body through various routes (fecal-oral for HAV and HEV; blood and body fluids for HBV, HCV, and HDV). They then target hepatocytes, the primary cells of the liver, which leads to the initial phase of infection. 2. *Immune Response and Inflammation:* The body’s immune system recognizes the viral infection and mounts a response. Infected hepatocytes present viral antigens on their surface, attracting immune cells like cytotoxic T lymphocytes. 3. *Acute vs. Chronic Infection:* *Acute Infection:* Characterized by rapid onset of symptoms such as jaundice, fatigue, and elevated liver enzymes. In most cases, especially HAV and HEV, the infection resolves spontaneously with the clearance of the virus. *Chronic Infection:* Particularly seen with HBV and HCV, where the virus persists in the liver. Chronic inflammation leads to liver fibrosis (scarring), cirrhosis (severe scarring and liver dysfunction), and can progress to liver cancer over time. 4. *Liver Damage Mechanisms:* *Direct Viral Cytopathic Effect:* Some hepatitis viruses can directly damage hepatocytes. *Immune-Mediated Injury:* The primary cause of liver damage, where the immune system's response to the infected cells leads to inflammation and cell death. #### Clinical Manifestations 1. *Acute Hepatitis:* Symptoms include jaundice (yellowing of the skin and eyes), dark urine, fatigue, nausea, vomiting, abdominal pain, and elevated liver enzymes. Most common with HAV and HEV, which do not typically lead to chronic infection. 2. *Chronic Hepatitis:* Often asymptomatic initially or with non-specific symptoms like fatigue. Progresses to more severe liver disease symptoms as fibrosis and cirrhosis develop, including ascites (fluid accumulation in the abdomen), hepatic encephalopathy (brain dysfunction due to liver failure), and variceal bleeding (bleeding from varices, which are enlarged veins). #### Diagnosis and Treatment 1. *Diagnosis:* Blood tests for liver enzymes (ALT, AST), bilirubin, and specific viral markers (antibodies and viral RNA/DNA). Imaging studies (ultrasound, CT, MRI) to assess liver damage. Liver biopsy in certain cases to evaluate the extent of fibrosis and inflammation. 2. *Treatment:* *Acute Hepatitis:* Mainly supportive care; specific antiviral treatments are rarely needed. *Chronic Hepatitis B and C:* Antiviral medications to suppress viral replication and reduce liver inflammation and fibrosis. *Hepatitis A and B Vaccines:* Available for prevention. *Liver Transplant:* In cases of end-stage liver disease or liver cancer.